There is no doubt that significant effort goes into expanding vaccination reach, especially to the last mile and by extension, Universal Health Coverage (UHC). One critical aspect of this process is definitely the supply chain process that ensures the right vaccines reach the last mile when needed and in the most potent conditions.
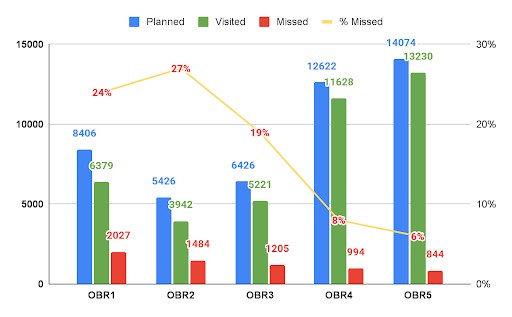
Vaccines are highly sensitive to temperature variations, including heat, light, and even excessive cold. This makes its delivery especially to underserved remote communities utmostly critical to the general immunization process. Over the last decade, eHealth Africa, with support from Sokoto State Government, Gates Foundation, and Dangote foundation has facilitated the delivery of over 10 million vaccines and dry goods across over 351 Primary Healthcare facilities in the 23 Local Government Areas of Sokoto State.
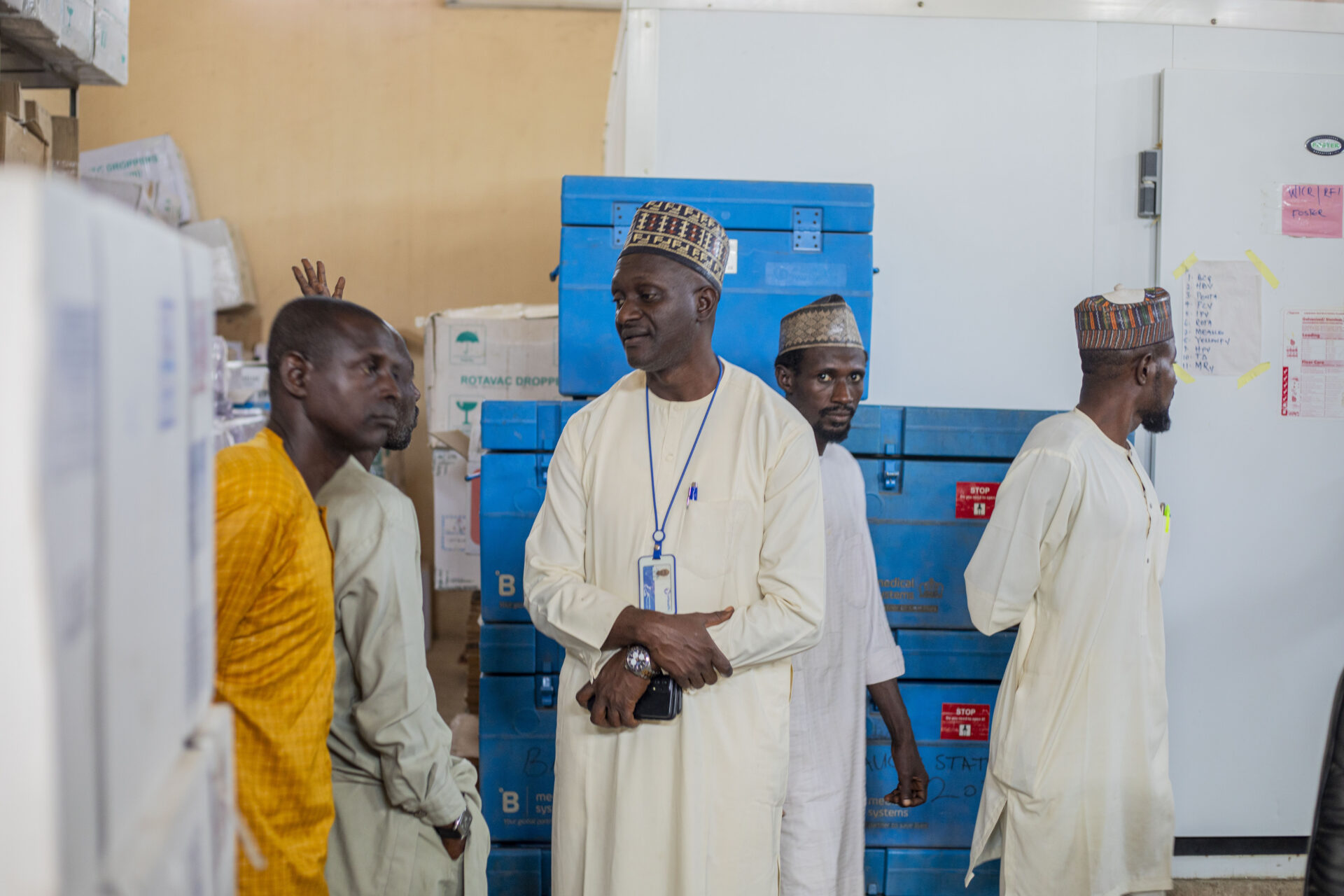
In a bid to replicate the impact in Sokoto state across other locations, eHealth Africa recently conducted a comprehensive high-impact capacity building for Direct Vaccine Delivery and Cold Chain officers in Bauchi state. These sessions revealed that delivering vaccines to underserved communities goes beyond moving vaccines from one place to another. Cold Chain officers and delivery officers were exposed to the deployment of digital tools for better accountability and ensuring that, indeed, all vaccines that got to PHCs are safe for consumption.

The Program Manager, Disease Prevention and Monitoring, Abubakar Shehu, explained that the capacity-building session conducted by ehealth Africa in partnership with the state government and the Ministry of Health was inspired by the need to bridge existing vaccine delivery gaps in the state.
Abubakar Shehu said the session is critical not only for ensuring safe vaccine delivery but also for strengthening accountability and potency monitoring. He said, “As a leader in the immunization space with more than a decade of experience, eHealth Africa is exposing partners to important digital tools such as the Logistics Management Information System (LoMIS) and temperature monitoring devices to ensure vaccines reach the last mile and remain accessible to the children who need them most.”
. This, according to him, will go a long way in not just boosting vaccine delivery but bringing more eligible children into the immunization net.
Leading the capacity building session, eHealth Africa’s Sokoto Vaccine Direct Delivery Coordinator, Ahmadu Bello, revealed that some of the gaps identified are the absence of proper temperature monitoring during vaccine transit. He said, “Vaccines are picked up from the cold store and delivered to facilities, but what happens between the cold store and the facility is not recorded. This lack of accountability could endanger the vaccines. ”
He also pointed out inconsistencies in monthly delivery schedules. “We also observed an inconsistency in monthly delivery schedules. If delivery begins in the first week, it must remain consistent; otherwise, stock-outs may occur. To address this, we encourage coordination between the central cold store, the national level, and the Primary Healthcare facilities to ensure timely distribution”, he added
Another critical aspect of vaccine delivery that significantly impacts not only immunization services but overall community health is reverse logistics. Bello emphasized that it is not enough to routinely distribute vaccines to PHCs without carefully assessing actual demand. “Some locations require more medical supplies than others, so it is important to prioritize facilities experiencing higher demand rather than allowing vaccines to sit on shelves elsewhere and eventually expire,” he noted.
He also stressed that the proper disposal of used vials and other dry waste remains essential to prevent harm to health workers and community members. “These are key lessons participants have taken away and will cascade to the colleagues they work with,” he added.
If anything, the sessions have changed the perception of Vaccine delivery officers to understand how their role is directly linked to saving lives and expanding vaccination reach. Relishing the potential impact of the capacity building, state team lead for Vaccine delivery, Abubakar muhammad said, “Now we understand timely delivery reduces wastage and stock-outs. We also learned the importance of deploying temperature trackers”.
Muhammed reiterated that the capacity building is a major springboard for improved immunization services in Bauchi state, saying, “With this new knowledge gained, we will deliver vaccines on time and make sure each facility receives vaccines with potency and in good condition.”
In a similar vein, Pharmacist Muhammad Kabir Salisu, Assistant State Logistics Officer, revealed that his team learned how to maintain vaccine potency from national entry to facility delivery, saying they were introduced to tracking applications and temperature monitoring systems.
He emphasized the need for every personnel in the supply chain to take responsibility for protecting children from vaccine-preventable diseases. He stated, “If you are a health professional and a hospital is built in your community, you should understand it is not meant only for your community. If essential medicines are not delivered properly and a life is lost, that responsibility rests with you.”
He added, “The same applies to immunization. If you do not deliver safe vaccines to the last mile, you are failing the people. That is the message to my entire team.”
Through sustained investment in digital innovation, capacity strengthening, and last-mile delivery systems, eHealth Africa continues to bridge critical gaps in vaccine access and accountability. By combining technology, field expertise, and strong government collaboration, the organization is strengthening supply chains, improving vaccine potency monitoring, and enhancing delivery consistency across states. As these efforts deepen and expand, more communities are gaining reliable access to safe vaccines, reinforcing stronger immunization systems and healthier futures for children.