Azeez- Ayodele Fatimah Ayotemitide
Across many low- and middle-income countries (LMICs), health systems face a confluence of systemic challenges. They are constantly shifting under the weight of policy instability, significant financing gaps, pervasive infrastructural deficits, and complex social pressures. In these contexts, resilience is not a luxury. It is the only way a system survives.
Resilience means designing systems built rooted in local ownership – not just to function today – but to endure and thrive amid uncertainty. These are systems that remain operational despite shrinking budgets, shifting priorities, or leadership transitions; that welcome innovation as fuel rather than falter under its weight; and that become more robust, adaptive, and impactful the more they are used.
The realities facing health systems in LMICs are not theoretical. They show up in efficient ways: Health facilities without stable power, critical services dependent on paper-based systems, data scattered across siloed platforms, staff turnover that erases institutional memory, digital tools that falter the moment donor funding ends, solutions designed for reporting – not for people, and infrastructure that cannot withstand policy changes or economic pressures.
When these weak points collide, the result is predictable: progress stalls, innovation slows, and entire communities feel the impact. This is why resilience matters. A resilient system can survive these pressures and continue delivering care consistently, reliably, and equitably.
Why the GDHF 2025 Theme Matters
As the global digital health community prepares for the 2025 Global Digital Health Forum (GDHF), the theme, “Advancing Digital Health Solutions in Low- and Middle-Income Countries”, places resilience where it belongs: at the center of the conversation.
Digital health has enormous potential across LMICs, but only when the systems beneath it are strong. For instance, without stable power, reliable data, or community-level visibility, even the most advanced tools struggle to take root.
The GDHF is one of the few spaces where these realities are openly acknowledged, and LMIC voices shape the global conversation. The 2025 theme pushes us to think beyond innovation as a standalone objective and instead, focus on the environments where innovation must live.
As the executive director, Atef Fawaaz puts it, “Digital health only succeeds when the foundations beneath it are strong. GDHF gives us a space to show that resilience isn’t an abstract idea. It’s the power, data, and community structures we build every day to keep health systems moving.”
eHealth Africa’s work spans the interconnected layers of digital health. It goes beyond applications and dashboards to the foundations that make them viable: integrated data platforms, reliable operational systems, sustainable power for clinics, tools that empower health workers, and community-centered support structures.
Together, they form the backbone of self-reliant health systems that don’t wait for permission, funding cycles, or external validation to deliver. At GDHF 2025, eHealth Africa joins national ministries, African innovators, and committed global partners to contribute to this vision and help shape the future of digital health – led from within and built to last.
This year, eHealth Africa will co-host a private side session with Bay Area Global Health Alliance, REACH, and the Africa Hub for Innovation & Development, focusing on “Digital interfaces that influence health behaviour among adolescents in Kenya and beyond”.
The session will explore how youth-centered tools, including AI-powered avatars and digital personas, can strengthen engagement and improve health outcomes. It reflects the kind of collaboration required to build systems that evolve, respond, and improve over time.
Similarly, eHA will be spotlighting three impactful interventions/ solutions while exploring opportunities to build collaborations and strengthen partnerships to scale the impact of these interventions.
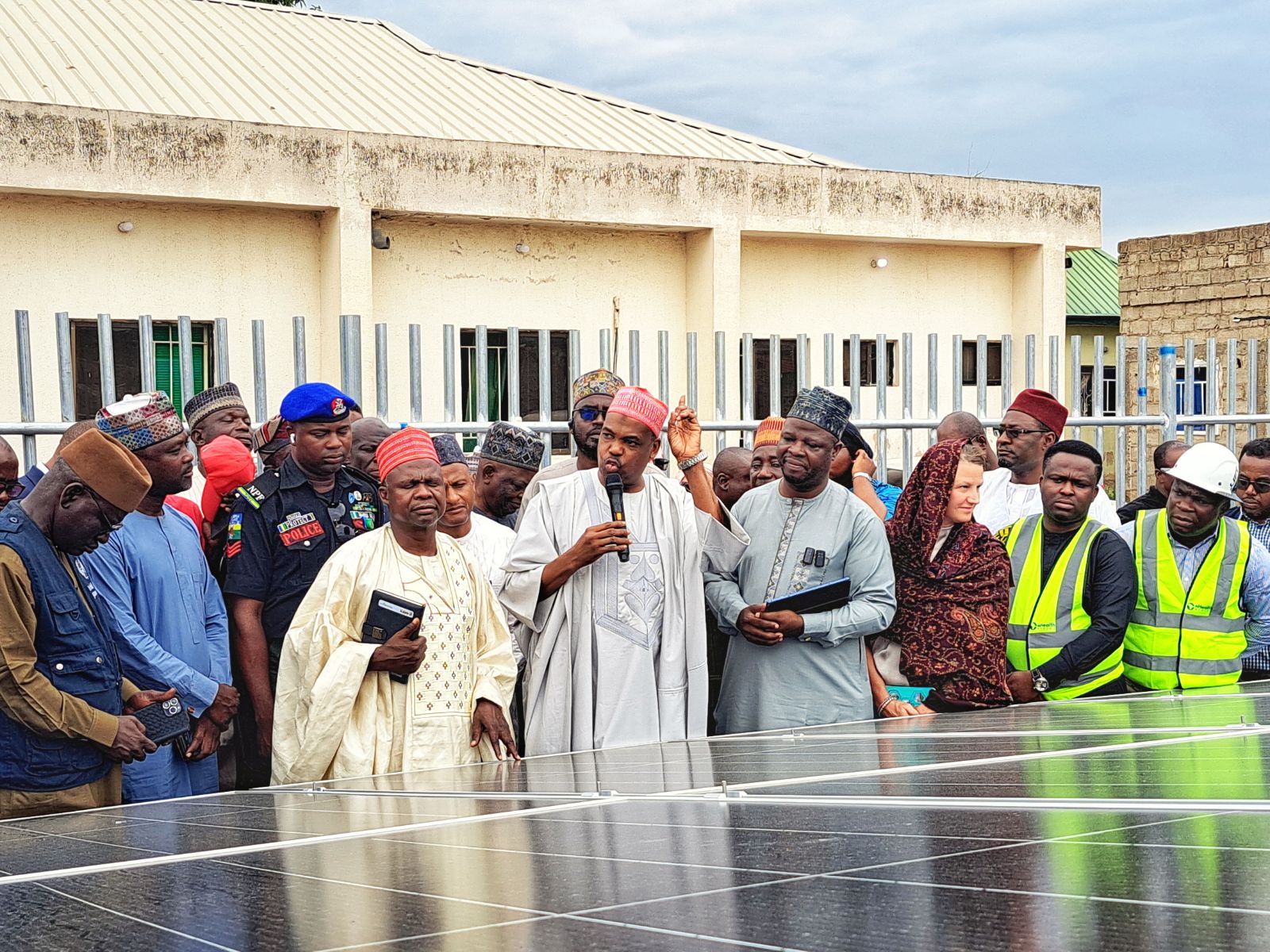
Solarization: Powering Reliability
Stable power is the backbone of digital health. Without it, cold-chain equipment fails, data cannot be entered or accessed, and facilities cannot deliver consistent service. eHealth Africa’s Solarization intervention provides sustainable energy to primary health centers, ensuring digital tools remain functional and essential services continue uninterrupted.
This intervention is a practical demonstration of resilience in action. So far, we have achieved 50+ self-powered PHCs toward a target of 238, simultaneously saving facilities over 2.5 million naira in fuel and maintenance costs. Scaling this impact is critical, as every self-powered facility represents a secure anchor for digital health, bringing consistent, life-saving care to underserved communities and reinforcing a scalable, transformative model of system durability.
PlanFeld: Turning Data Into Action
Resilient health systems require real-time visibility. Planfeld enables operational teams to track field activities, manage logistics, coordinate emergency response, and make informed decisions using live data.
A key highlight of its impact was in Kebbi State, where the tool was instrumental in developing 225 Ward-level Digitized Micro Plans for 21 Local Government Areas (LGAs), equipping over 2,950 teams with precise implementation schedules. Due to this success in strengthening planning and data utilization, the state government of Lagos subsequently invited eHealth Africa to deploy PlanFeld for microplanning across their system as well. It strengthens a system’s ability to adapt – one of the core functions of resilience.
CHAT: Community-Level Strength
This tool is integral to our work in climate adaptation. It was successfully piloted across 3 states and 30 Primary Health Centers (PHCs) in Nigeria. Building on this success, the next phase involves direct integration with DHIS2 and the addition of critical hazard areas, such as Heatwaves and Drought, into the assessment framework. By embedding comprehensive, data-driven routines and critical climate intelligence at the community level, CHAT ensures that system resilience is not merely confined to central planning or infrastructure, but is robustly supported by last-mile visibility and human capacity.
Collaboration in Focus: eHealth Africa at GDHF 2025
As eHealth Africa heads to GDHF 2025, the focus is not merely on presenting tools, but on advancing a conversation that matters. Importantly, we are out to take on bold conversations on how to build health systems that continue functioning and continue improving, no matter what challenges arise.
Resilience is not built in a day. It is built through intentional design, strong infrastructure, meaningful partnerships, and solutions that communities can trust and sustain. At GDHF 2025, eHealth Africa joins national ministries, African innovators, and committed global partners to contribute to this vision and help shape the future of digital health – led from within and built to last.