By Moshood Isah

Losing a child to a vaccine-preventable disease brings a pain that words can barely capture. For parents like Maman Fati, the grief is made even heavier by the knowledge that protection was once within reach. The memory of watching a child fade from an illness that could have been prevented is a lifelong burden that transforms sorrow into resolve, turning loss into a call to protect other children from the same fate.
Popularly known as Maman Fati (Fatima’s mother), Maryama Usman is a middle-aged resident of Ungogo Local Government Area in Kano State. “Refusing to vaccinate your child has huge consequences. I have experienced this firsthand and learned the very hard way, due to my negligence,” an emotional Maryam recalls, reflecting on the loss of her daughter to vaccine-preventable diphtheria.
Interestingly, Maman Fati was never a vaccine-defaulter. “I have always vaccinated all my children, but sadly, I missed the vaccination of this last child and we paid dearly with her demise.” Her only daughter who missed vaccination eventually succumbed to the illness a few months ago. “Before her death, my daughter battled chronic malaria, epileptic-like conditions, swelling and stiffness of the neck. She ultimately lost her battle to diphtheria because she had not been vaccinated,” she added.

Yet, Maman Fati did not allow grief to consume her. Instead, she renewed her determination not only to ensure that all her children and herself were vaccinated, but also that all eligible children in her community were protected. During the Human Papillomavirus (HPV) intensification campaign led by eHealth Africa in Kano State, Maryam actively ensured that eligible girls in her community received the HPV vaccine. “The myth that vaccination causes infertility in women is false. I vaccinated all my other daughters, and they are healthy, married, and giving birth to my grandchildren,” she emphasized.
Maman Fati has vowed to stay vaccinated herself and to consistently lead advocacy efforts to increase vaccination coverage in her community. “I am pleading with our women and caregivers to always take their children for vaccination,” she urged.
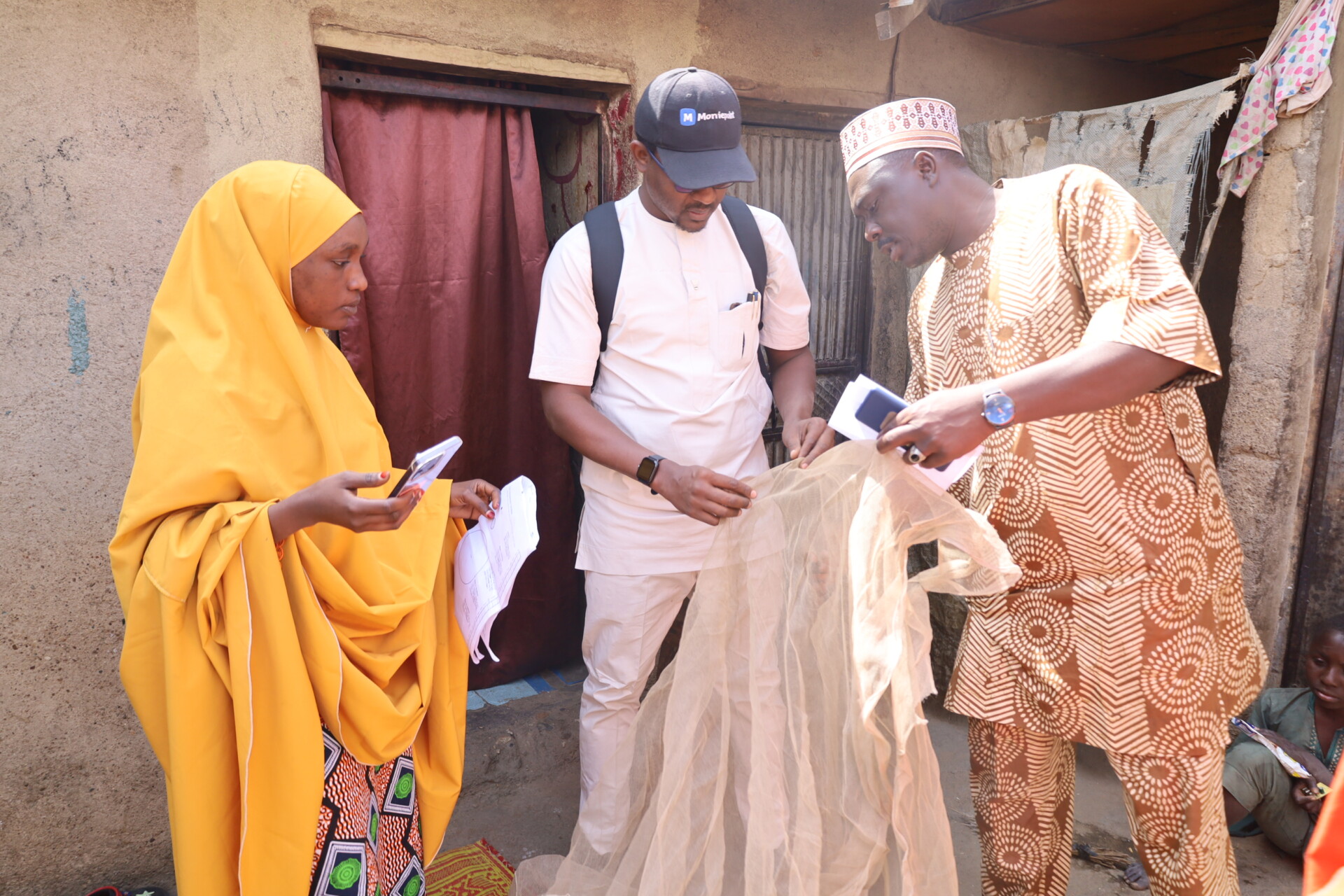
Her passionate plea was preceded by a co-created awareness campaign on HPV vaccination, led by eHealth Africa and supported by United Nations Children’s Fund (UNICEF) in Kano and surrounding areas. The awareness sessions targeted caregivers, state and LGA gatekeepers and Routine Immunization providers educating them about the dangers of HPV, particularly for girls aged 9–11 years. After thesessions eHealth Africa team immediately conducted a strategic HPV intensification vaccination in schools and communities especially for young girls of 9-years old.
The Project Manager, Salahudeen Sambo, noted that his team followed the awareness sessions with an intensive HPV vaccination campaign across communities. “We have observed a shift in behavior among caregivers and community members; from skepticism about vaccination to a strong demand for vaccines. Currently we are even experiencing vaccine stockout for HPV in Kano and Bauchi state. Thus, we call on all stakeholders to continue supporting efforts to protect young girls from HPV so they can lead healthy lives,” he said.
UNICEF has consistently emphasized that the HPV vaccine is safe and effective, protecting against HPV, the most common sexually transmitted infection (STI) worldwide and a leading cause of cervical cancer. The vaccine helps prevent cancers and genital warts caused by the virus and is recommended for children from 9 to 26 years of age. Early vaccination is essential to protect children before exposure to the virus.
Maman Fati’s story is a powerful reminder that loss can fuel change. From personal tragedy, she has become a beacon of hope and action, ensuring that no other child in her community suffers the same fate. Her courage and advocacy highlight the lifesaving power of vaccines and the profound impact one determined individual can have in safeguarding the health of an entire community.