Tijesu Ojumu
Vaccines have long been one of humanity’s greatest health success stories. They’ve helped us wipe out deadly diseases, keep children healthy, and respond to emergencies like the COVID-19 pandemic. But what happens when vaccines don’t reach the people who need them?
Across many parts of Africa, health workers face an invisible challenge: vaccine wastage. This occurs when vaccines are lost, spoiled, or expire before they can be used. Sometimes, it’s because of unreliable power, poor storage, or long travel delays. Other times, it’s simply because more vaccines were sent than were needed and by the time they’re opened, they’ve already gone to waste.
For communities where every dose counts, vaccine wastage doesn’t just cost money. It costs trust. And lives. This was the focus of a powerful Insights Webinar hosted by eHealth Africa, where public health leaders, field experts, and digital health innovators came together to ask one question:
How can we make sure every vaccine reaches the people it was meant for, safely and on time?
The Problem: Wasted Doses, Missed Opportunities
When we think about vaccines, we often picture the jab, the moment of protection. But getting a vaccine to that moment involves a long, delicate journey: it must be stored at just the right temperature, tracked across distances, and kept safe until the moment it’s used.
In this journey, a lot can go wrong. One speaker at the webinar described how even a short power outage can spoil an entire batch. Another explained how, in some remote clinics, health workers open a vial expecting 10 children to show up but only 2 come. The rest of the doses? Tossed out. These are not rare issues. In fact, it’s estimated that up to 50% of vaccines can be wasted globally if systems aren’t strong.

The Good News: Smarter Tools Are Making a Difference
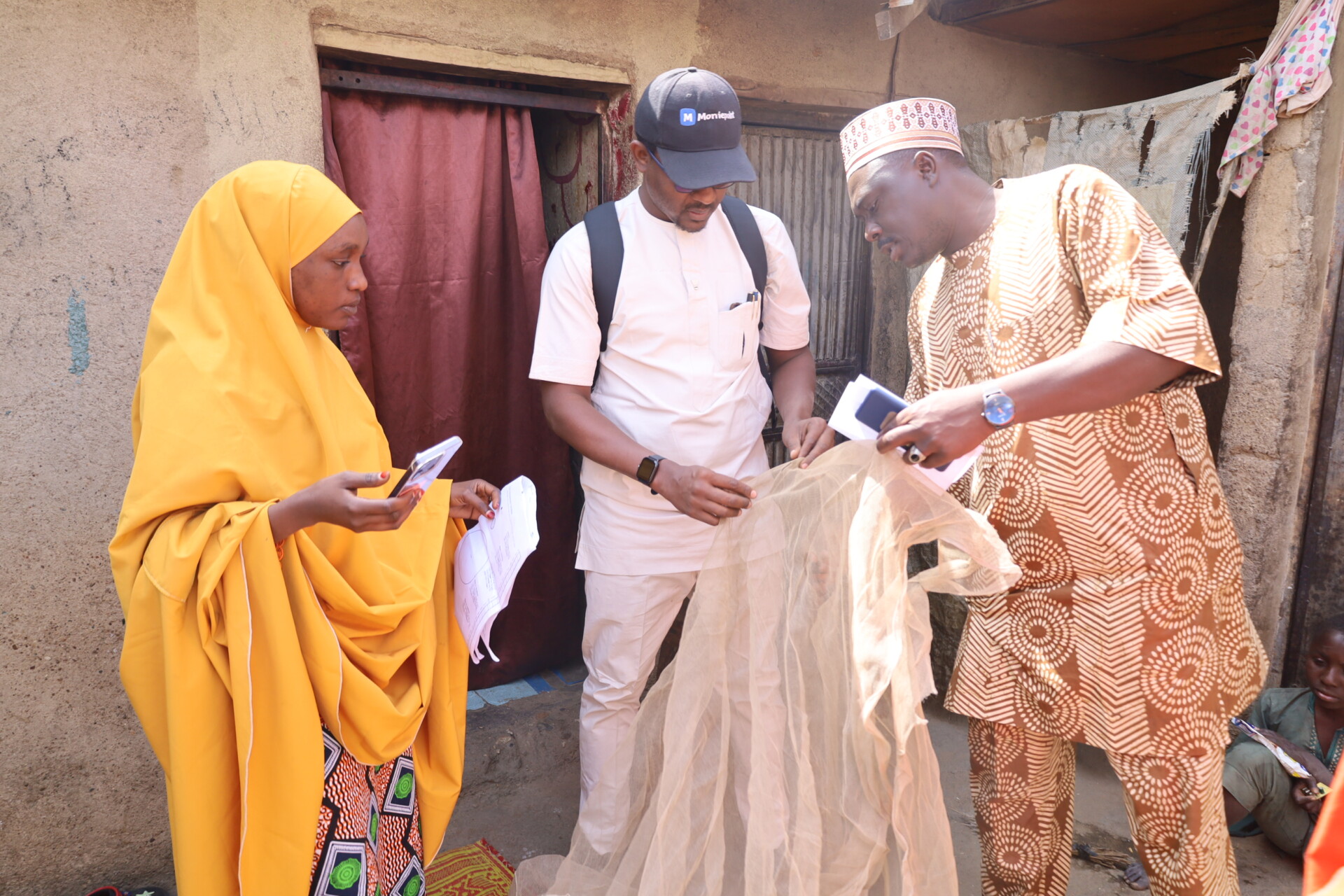
While the challenges are real, so is the progress. Across Nigeria and other African countries, digital solutions are helping health workers plan better, respond faster, and waste less.
Take Planfeld, for example, a tool developed by eHealth Africa. It helps local teams map out exactly where people live, how many doses are needed in each area, and how to deliver them efficiently. With better planning, fewer doses go to waste.
There’s also the rise of real-time temperature sensors. These small, smart devices sit inside vaccine coolers and alert health teams if temperatures become unsafe. That way, problems can be fixed before vaccines spoil. In areas without reliable electricity, solar-powered fridges are a game changer. These eco-friendly units are keeping vaccines safe in even the most remote villages.
Innovation Doesn’t Stop at Technology
Not all solutions are high-tech. In fact, some of the most effective fixes are surprisingly simple. Health workers shared stories of success from the field: planning vaccination days to match market days, making reminder calls to parents, checking expiry dates more often, and involving local leaders to boost turnout. Some clinics even use WhatsApp to coordinate last-minute deliveries between sites. “Digital systems are powerful,” one speaker said, “but it’s the people behind them who make them work.”
Why It Matters: Trust, Safety, and Equity
Reducing vaccine wastage isn’t just about numbers on a spreadsheet. It’s about protecting lives and building trust in healthcare systems. When people see vaccines are handled carefully, they feel safer getting them. And when health workers are supported with the right tools, they can serve their communities with confidence. There’s also an issue of fairness. Every wasted dose is a missed chance to protect someone often in communities that already struggle with access. Smarter systems help ensure no one is left behind.
What’s Next?
The panelists ended the webinar with a clear message to governments, donors, and the public:
We must invest not just in vaccines but in the systems that deliver them. That includes:
- Training for frontline health workers
- Digital tools for planning and tracking
- Cold chain infrastructure like fridges and coolers
- Community engagement to reduce missed appointments
When we do this, we don’t just reduce waste. We increase impact.
One Dose at a Time
Africa is leading the way in turning vaccine challenges into opportunities for innovation. From the use of AI to plan smarter routes, to mobile clinics reaching the last mile, these efforts are not just saving money — they’re saving lives. Because behind every successful vaccination is a system that worked. A nurse who planned ahead. A delivery that was on time. A fridge that kept running. And a child who will grow up healthy, all because one dose made it through.
Let’s make sure every dose does.
Learn more about these efforts at ehealthafrica.org