Tijesu Ojumu

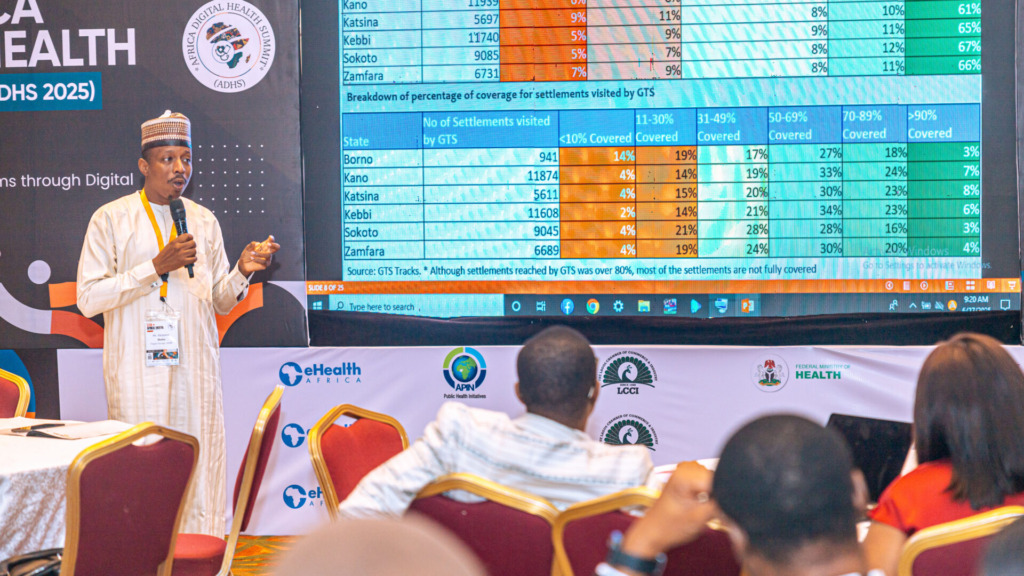
At the 2025 Africa Digital Health Summit (ADHS) in Lagos, eHealth Africa had the privilege of hosting a side session on a topic of growing urgency: The Role of Digital Innovation in Advancing One Health in Africa.
The session brought together health experts, environmental scientists, animal health professionals, and digital innovators for one clear purpose: to explore how a more connected, data-driven approach can strengthen our ability to predict, prevent, and respond to health threats that cross sectors and species.
The One Health approach recognizes that the health of people, animals, and the environment are deeply interconnected. In a continent where zoonotic diseases are common, food security is vulnerable to climate shifts, and health systems are often fragmented, a siloed approach simply doesn’t work. If we want to control disease outbreaks, we can’t wait until humans are affected. We have to monitor the animals, the environment, and the social systems surrounding them.
This is where digital innovation comes in.
At eHealth Africa, we’ve seen the value of tools like geospatial tracking systems for disease surveillance, digital microplanning platforms like Planfeld, and integrated data dashboards that offer real-time visibility into emerging health threats. But what truly stood out in the ADHS conversation was this: technology alone is not enough.
Speakers across the session emphasized that digital tools only work when they’re part of a broader ecosystem that includes trust, interoperability, local engagement, and strong multisectoral coordination. One of the key takeaways was the need to design systems that are inclusive—tools that work not just for human health, but also for veterinary services, environmental monitors, and community-based responders.
Several powerful insights emerged:
- Data Quality & Ownership: Without high-quality, context-rich data that is owned and trusted by local actors, digital tools will never achieve their full potential.
- Workforce Readiness: Intersectoral collaboration only works when human capacity is strengthened across the board. This includes training veterinarians, environmental scientists, and frontline health workers to engage with shared systems.
- Inclusive Infrastructure: It’s not enough to have the tech; systems must be built to work across rural and urban settings, among both literate and non-literate populations, and in regions with limited internet connectivity.
- Impact Beyond Tools: As one speaker noted, “Success is not a shiny new dashboard. Success is when an outbreak is stopped before it spreads.” That’s the standard we must hold innovation to.
For eHealth Africa, this session was not just about sharing our work—it was about listening, learning, and reinforcing our commitment to support African governments and partners with digital tools that make sense locally and can scale regionally.
This is why we are investing in interoperable systems, building relationships across sectors, and focusing on solutions that don’t just react to emergencies but build long-term resilience.
As we left the ADHS 2025 summit, one thing was clear: Africa doesn’t need more tech for tech’s sake. It needs systems that reflect our realities, connect our knowledge, and protect our communities.
The One Health approach offers a framework for that kind of transformation—and digital innovation, when done right, can help bring it to life.
Let’s build those systems together. To explore eHealth Africa’s One Health work and digital health partnerships, visit ehealthafrica.org or follow @eHealthAfrica across all social media channels.