By Sadiq Haruna Hassan
A child in Kano State getting vaccinated
Every year, Nigeria spends millions of dollars to procure vaccines. The amount has grown from over US$ 302 million in 2015 to an estimated US$ 426.3 million in 2020. 1 Once the vaccines have been procured, a major challenge is maintaining the cold chain in transit to and on-site at last-mile health facilities. The cold chain is the system of storing and transporting vaccines at recommended temperatures—ideally between 2°C and 8°C—from the point of manufacture to the health facilities where they are used.2 If the cold chain is broken at any point between manufacture and usage, it could result in:3
Loss of vaccine potency
High vaccine wastage rates
Loss of funds spent on procuring vaccines
Need for re-immunization
To maintain the cold chain, health facility workers, and cold chain officers at local government and state levels in Nigeria must monitor and track the performance of cold chain equipment (CCE) regularly. Health workers record data on daily temperatures of CCE and the functionality of the equipment at health facilities across the country ( i.e. whether the equipment is working or not) using paper-based charts and forms, and cold chain officers visit health facilities routinely to collect this data.
A vaccinator in Kogi State shows us the vaccine to be used in her House-to-House Immunization Plus Days visit
As a result of insecurity, the location of the health facilities, and now, the COVID-19 pandemic, conducting this process in Northern Nigeria has been challenging.
Vaccine Direct Delivery is a third-party logistics (3PL) service offered by eHealth Africa to the Sokoto and Zamfara State Primary Health Care Management Boards. Through this service, eHA picks up the required amount of vaccines from the state cold stores, transports them at the appropriate temperatures, and delivers directly to health facilities that are equipped with functional CCEs, ensuring that the cold chain is maintained and that the vaccines remain potent even in transit. In addition, using the VARO application, eHA helps decision-makers and key stakeholders to remotely monitor the performance of CCEs at 393 apex health facilities in both states.
A Health Delivery Officer in Zamfara State downloads the temperature records of Cold Chain Equipment
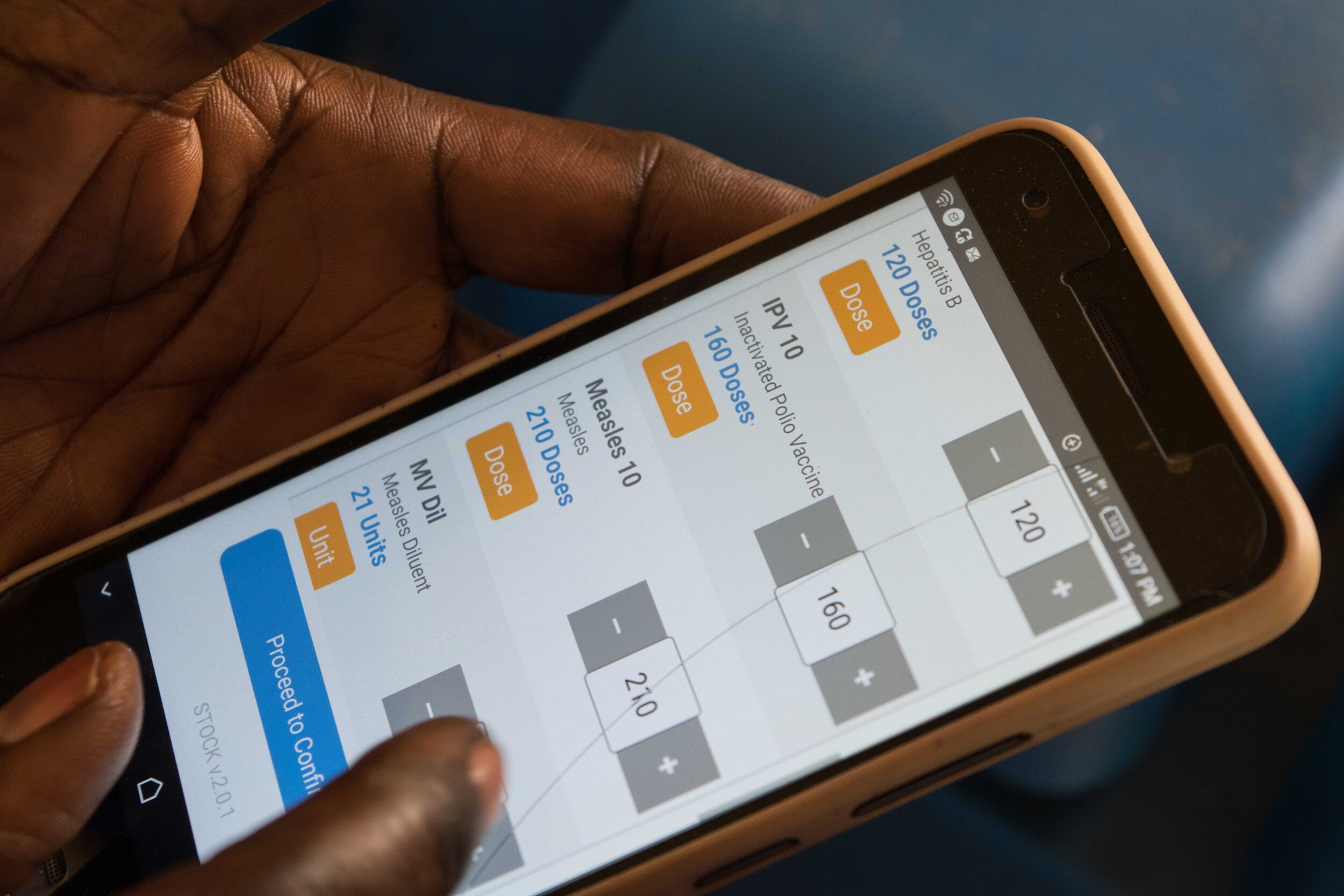
In Kano state where VDD is not operational, the apex health facilities, LG, zonal, and state cold stores keep track of CCE performance using LoMIS Stock, a solution developed by eHealth Africa. The solution allows health workers to send reports about vaccine stock data including vaccine utilization, wastage, and cold chain equipment functionality, using their mobile phones. These reports can be accessed in near-real-time by cold chain officers and decision-makers so that the faulty cold chain equipment can be fixed and back-up protocol for maintaining the cold chain can be followed.
Vaccines save lives. At eHA, our goal is to provide our partners with accurate data and technological tools so that they can better reach underserved populations with potent life-saving vaccines.